ICU Chest Films > Fluid in the Chest > Pulmonary Edema
Pulmonary Edema
![]()
Pulmonary edema occurs when fluid traverses capillary membranes and enters the alveolar space. It is the most common cause of decreased oxygenation in the ICU patient.
Three mechanisms lead to pulmonary edema. These are:
1. Increased hydrostatic gradient
2. Diminished oncotic pressure
3. Increased capillary permeability due to endothelial injury
Any one or more often a combination of these mechanisms will cause fluid to enter the alveolar space. The causes of pulmonary edema are broadly catogorized as cardiac versus non-cardiac. Poor cardiac function will cause increased hydrostatic pressures in the pulmonary capillary bed resulting in cardiogenic pulmonary edema. Non-cardiogenic pulmonary edema can result from volume overload due to renal failure, over hydration, or from diminished oncotic pressure in the liver failure patient, or from endothelial injury as in the patient with ARDS. The radiographic manifestations of cardiogenic edema (much more common) are shon on the next several pages.
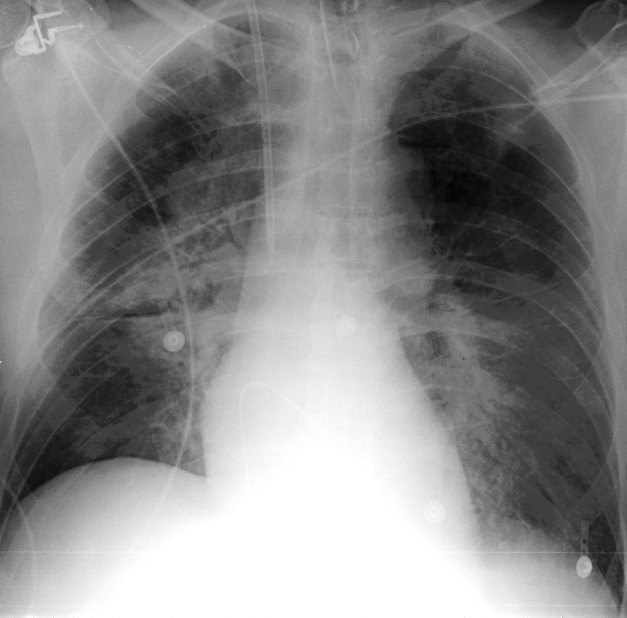
This is a patient with pulmonary edema with typical bilateral "batwing"
increased pulmonary vasculature.